
Reminiscence Therapy for Dementia
High-quality dementia care must do more than support day-to-day needs—it should actively promote emotional wellbeing, protect dignity, and preserve the individual’s sense of identity, even as cognitive changes progress. For care professionals and families alike, finding an approach supporting clinical needs and meaningful connection is essential.
Reminiscence therapy has long been recognised as a valuable, person-centred intervention within dementia care. Backed by NICE guidance and supported by the Alzheimer’s Society and Dementia UK, it focuses on engaging long-term memory through sensory prompts, personal storytelling, and shared experiences. This can help reduce anxiety, ease social withdrawal, and enhance a person’s confidence, particularly in the earlier to moderate stages of dementia.
At our care home, reminiscence therapy is not a one-off activity but a thread that runs through everyday interactions, from life story work at admission to gentle conversations over tea. Staff are trained to use reminiscence as a therapeutic tool and as a means of getting to know each resident, essential for tailoring care in line with their values, history, and wishes.
Understanding How Dementia Progresses
Dementia is a progressive condition, and as it advances, the care a person needs must evolve too. While symptoms and rate of progression vary, many individuals experience changes in memory, language, reasoning, and emotional regulation over time. Understanding these shifts is key to providing care that remains both appropriate and respectful at every stage.
In the early stages, individuals may still express themselves well, participate in conversations, and engage in familiar activities. This is often the best time to introduce life story work and reminiscence therapy, building a strong foundation for personalised care. As memory becomes more impaired, those earlier conversations and insights continue to guide carers in responding to emotional cues and maintaining the person’s sense of identity.
As the condition progresses into the moderate and later stages, people may experience difficulties with decision-making, spatial awareness, and communication. At this point, the consistency of relationships, the use of familiar sensory prompts, and a calm, responsive approach become increasingly important. Reminiscence therapy can offer moments of clarity or recognition, even when verbal language is limited, creating a space where the person feels safe, known, and reassured.
Care that is informed by an understanding of dementia’s trajectory doesn’t simply respond to decline—it anticipates changes and adapts with compassion. It draws on what matters most to the individual: their history, their routines, and their relationships. Clinical professionals referring into care settings need the confidence that these principles are embedded in daily practice, not just in documentation, but in the way residents are spoken to, supported, and valued.


A Person-Centred Approach to Reminiscence Therapy
Reminiscence therapy is an established, non-pharmacological intervention used in dementia care to support wellbeing, communication, and emotional connection. It involves engaging a person through memories and familiar experiences, often using prompts such as music, photographs, personal belongings, or scents. While it is not designed to improve memory function, its strength lies in its ability to connect individuals with their sense of self, even as short-term recall fades.
Long-term memory often remains more intact in the earlier stages of dementia, so drawing on past experiences can help the person feel more grounded and secure. For example, a familiar song from the 1950s may spark a moment of recognition or encourage someone to sing along, even if verbal communication has become difficult in other contexts. These small moments can lift mood, reduce anxiety, and foster trust between residents and staff.
Reminiscence therapy is most effective when it’s not treated as a standalone activity, but rather woven into the culture of care. In a care home, reminiscence therapy is integrated into structured sessions and daily interactions. These might include themed group activities based on a resident’s era of interest, or simply a one-to-one chat over tea using a memory box filled with personal keepsakes. These exchanges can provide meaningful insight into a person’s background, guiding staff in offering care that is not only clinically appropriate but also emotionally attuned.
Staff are trained to deliver reminiscence in a way that respects each resident’s abilities, preferences, and boundaries. It’s not about testing memory or focusing on what’s been lost, but rather about creating a safe space for expression, connection, and dignity. For residents living with more advanced dementia, sensory-based reminiscence using scent, texture, or music can be particularly effective when words are no longer accessible. It supports not just emotional wellbeing but continuity of identity—something every person living with dementia deserves to hold on to.
Involving Families in Reminiscence Therapy
Families are often the most valuable source of insight when it comes to supporting someone living with dementia. They hold the details of life stories, cherished routines, and meaningful moments that can be used to tailor care. Involving families in reminiscence therapy not only strengthens the person’s sense of identity but also offers relatives a positive, engaging way to maintain connection, even when communication becomes more difficult.
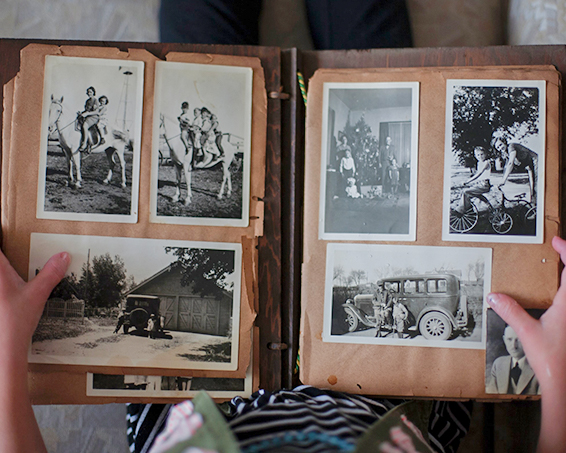
At our care home, we actively encourage families to contribute to reminiscence work through conversations, sharing old photographs, or helping build a personal memory box. These items are more than keepsakes—they are prompts for conversation, storytelling, and shared understanding. Familiar voices recalling familiar stories can offer immense reassurance to a person with dementia, especially during periods of disorientation or anxiety.
This collaborative approach also helps care teams develop a fuller picture of the individual. Knowing what school someone went to, the job they loved, or their favourite holiday destination doesn’t just inform activity planning—it shapes how we speak to them, what we place in their room, and how we support their daily routines. Being part of this process can be a comfort for families. It offers a sense of purpose and a practical role in their loved one’s care journey. Reminiscence therapy can also ease some of the emotional strain that often accompanies dementia by creating moments of recognition, laughter, and closeness, especially in the earlier stages of the condition. Families may need guidance too, which is why carers tend to be on hand in a care home to offer suggestions, explain how reminiscence therapy works, and show how it can be gently introduced at home or during visits. Even short conversations about a wedding day, a favourite pet, or a classic film can have a real impact on wellbeing.

Life Story Work in Building the Foundation for Personalised Care
Life story work is a key component of person-centred dementia care. It involves collecting and recording details about a person's background, relationships, values, and life experiences, often in a format such as a book, folder, or digital profile. Unlike reminiscence therapy, which focuses on stimulating memory in the moment, life story work serves as an ongoing reference point, supporting carers, clinicians, and families in understanding the person beyond their diagnosis. A well-developed life story can inform every aspect of care, from how we structure a person’s daily routine to the language we use and the activities we offer. For someone who once worked as a gardener, time outdoors or handling soil may provide calm and connection. For another, music from their youth may offer emotional comfort, even if they can no longer express why.
Life story work usually begins as part of the admissions process, but it doesn’t end there. Families are encouraged to continue contributing memories, photographs, and anecdotes, and our team adds to each resident’s story over time. This shared effort helps staff respond not just to behaviour or need, but to the person’s unique character and life journey. It also means care plans are rooted in the individual’s values and preferences, not just their medical profile. This approach aligns closely with national best practice guidance. Both NICE and SCIE advocate for life story work as part of delivering meaningful, personalised dementia care. It supports continuity, enhances communication, and helps staff provide emotional reassurance when residents are distressed or disoriented. It can also be an invaluable tool in decision-making, helping carers and professionals understand what matters most to the person.
For families, life story work offers a way to remain involved, especially as their loved one’s condition progresses. Contributing to someone’s story brings a sense of purpose and preserves memories that might otherwise fade from everyday conversation. For clinical professionals, it’s a reassurance that referrals are being made into a setting where personhood is truly at the centre of care.
Local Services and Support
Supporting someone with dementia is rarely something one person—or one organisation—can do alone. Effective care requires a support network, including families, health and social care professionals, and specialist services. Knowing where to turn for help, both practically and emotionally, can make a significant difference for carers and families, especially when navigating complex or changing needs. Across the UK, a range of services exist to support people living with dementia and those who care for them. These include memory clinics, dementia support workers, occupational therapists, and community mental health teams. Many areas also offer day centres, respite care, and support groups that help prevent isolation and provide carers with valuable breathing space.
Care homes work closely with local healthcare providers, including GPs, district nurses, and dementia specialists, to ensure continuity of care. We also signpost families to trusted services such as Dementia UK’s Admiral Nurse helpline, Age UK, and local social care teams who can offer advice on funding, legal matters, and access to community support. This collaborative approach helps to build a safety net around both the individual and their family. Whether a person is transitioning into full-time care or still being supported at home, early engagement with local services helps create a care plan that is proactive rather than reactive.
For professionals, working in partnership with a care home that values these connections offers peace of mind. You can be confident that referrals will be followed up, information shared appropriately, and families supported to access the wider resources available to them. It’s all part of a holistic approach that recognises dementia as a health condition that affects every aspect of life.
Dementia Care That Connects Past and Present
Reminiscence therapy, life story work, and thoughtful, individualised care strategies are more than just techniques, they are how we ensure that every resident at Manor House Care Home in Stafford continues to feel seen, valued, and safe. For families, this approach brings comfort. For professionals, it offers confidence that referrals are being made into a setting that understands the clinical, emotional, and human dimensions of dementia care.
If you're looking for specialist dementia care in Stafford that supports each person’s identity, wellbeing, and dignity at every stage, we warmly welcome you to get in touch. Our team would be happy to talk through your needs or arrange a visit. Contact us today to learn more about dementia care at Manor House Care Home in Stafford, or to arrange a private tour and discussion with our care team.
References
National Institute for Health and Care Excellence (NICE)
NICE Guideline [NG97] Dementia: assessment, management and support for people living with dementia and their carers https://www.nice.org.uk/guidance/ng97
Alzheimer Scotland, Reminiscence Therapy, https://www.alzscot.org/living-with-dementia/getting-support/accessing-alzheimer-scotland-support/therapeutic-activity/reminiscence-therapy
Dementia UK, Meaningful activities for a person with dementia: https://www.dementiauk.org/news/meaningful-activities-for-a-person-with-dementia/
